Medical Students
Announcements
Week 3. February 9-13, 2026
Tuesday, February 10
4:00 PM | Urology- Dr. Judge| Library 1
5:00 PM | Vascular - Dr. Wang | Library 1
Thursday, February 12
12:00 PM | Hifidelity Simulation - Dr. Hallagan | Brighton Sim Center
Block Schedule
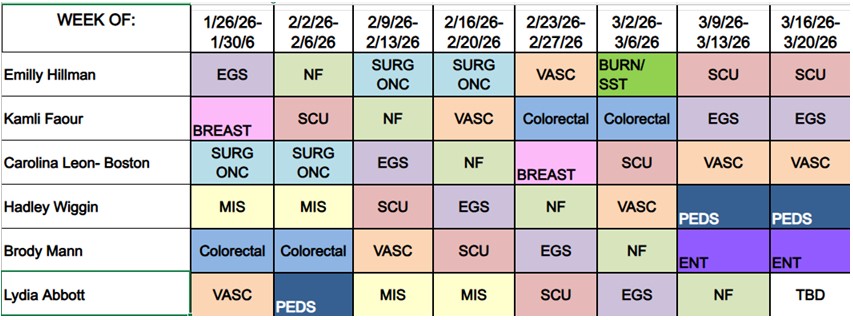

Table of Contents
Structure of Clerkship
Surgical Service Descriptions
- Breast
- Colorectal
- Emergency General Surgery (EGS)
- Minimally Invasive Surgery (MIS)
- Pediatric Surgery
- Surgical Intensive Care (SCU)
- Surgical Oncology
- Thoracic
- Trauma
- Urology
- Vascular
- Helpful Documents
Requirements
The following are due by the end of the rotation:
- Surgery Doc cards (2)
- Surgery Pain DOC card (1)
- Written H&P (3)
- Diagnostic Assessment/Reasoning Tool (DART) (1)
- Oral presentation (Timing TBD)
- Case logs (60)
Structure of the clerkship
1 week rotations
These rotations are meant to expose you to the breadth of surgery. One week can feel short but you should be able to see a selection of representative cases and disease processes. It is critical to start the week ready to go. You should know where and when to meet your team before the first day. Please review the service descriptions at the end of this document.
2 week rotations
You will be assigned to one of the “core” surgery services for 2 weeks during your clerkship. The goal is to allow you to see a variety of patients from start to finish. You will also get to spend a longer time with attendings and residents on the service
Call/Nightfloat
You will take call with the on-call resident team. Generally call teams are comprised of 4 residents. A chief resident (R4 or R5), a consult resident (R2 or R3), a SCU resident (R2) and an Intern (R1). You will join this team for the entire shift and your assignments and responsibilities will be assigned by the chief resident. You should expect to see an assortment of emergency general surgery consults and trauma activations as well as a variety of operative cases.
Daytime call
Daytime call starts at 6am and ends at signout (6:30pm). Find out who is the chief resident for the day you are on call (Amion.com) and contact them for instructions on where to meet. Depending on what is going on, you may be sent straight to the OR or you may join a team to help round on the floors.
Night float
Night float begins Sunday night at 6pm and ends Saturday morning at 6am. You should stay until you are excused each night.
Service Descriptions
Breast
The breast rotation will give students an immersion in both benign and malignant breast surgery. You will have the opportunity to see complex interdisciplinary and shared decision making in the office as well as the surgical care of these disease processes. Most of your time will be at the Breast Care Center and Scarborough Surgery Center so be prepared to travel.
Outpatient office: 100 Campus Dr Suite 121, Scarborough, ME 04074
Students should spend at least one half day at the office during the week. Timing should be arranged with your team.
Common diagnoses/cases:
- Breast cancer
- Benign breast disease
- Lumpectomy
- Mastectomy
- Sentinel node biopsy
- Breast reconstruction
Burn / Skin Soft Tissue
The burn service cares for a variety of urgent and elective burn patients. They also see a variety of consults for skin and soft tissue pathologies among in patients.
Common diagnoses/cases:
- Burns
- Burn excision and grafting
- Skin flaps
- Reconstruction
- Necrotizing soft tissue infections (NSTI)
- Decubitus ulcers
Colorectal
This group cares for a variety of colon and rectal diseases. You will be exposed to large open, laparoscopic and robotic colon resections as well as a variety of anorectal pathologies.
Outpatient office: 55 Spring St. Scarborough ME 04074
Students should spend at least one half day at the office during the week. Timing should be arranged with your team.
Common diagnoses/cases:
- Colon and rectal cancer
- Diverticulitis
- Ulcerative colitis
- Crohns
- Hemorrhoids
- Fissure
- Anal Fistula
- Rectal prolapse
Emergency General Surgery (EGS or ACS)
This service is one of the core experiences in general surgery. It serves as the primary, non-subspecialty service for all general surgery consults and admissions. Here is where you will encounter all of the “bread and butter” emergency operations and disease processes.
Outpatient office: 887 Congress St. Suite 400, Portland ME 04102
Students are NOT required to attend office while on EGS but are encouraged to join one of the general surgeons as scheduling allows
Common diagnoses/cases:
- Appendicitis (appendectomy)
- Cholecystitis, cholangitis, pancreatitis (cholecystectomy)
- Small bowel obstruction (lysis of adhesions)
- Diverticulitis (Sigmoid colectomy, Hartmann’s procedure)
- Ischemic colitis
- Crohns
- incarcerated/strangulated hernia
- Enterocutaneous fistula
- Skin soft tissue abscesses
ENT
Outpatient office:
Students should spend at least one half day at the office during the week. Timing should be arranged with your team.
MIS
You will primarily be assigned to our Minimally Invasive Surgery (MIS) service. This service provides care to a wide variety of patients and uses advanced techniques in robotic, laparoscopic and endoscopic surgery.
Students should spend at least one half day at the office during the week. Timing should be arranged with your team. Dr. Brady welcomes students to his office on Monday afternoons- check with your team to see if this will work out.
Common diagnoses/cases:
- Bariatric Surgery (sleeve gastrectomy, gastric bypass)
- GERD
- Hiatal Hernia
- Ventral hernias
Pediatric Surgery
Pediatric surgery is an incredibly varied and valuable educational rotation. Here you will see a wide spectrum of pediatric surgical disease.
Outpatient office: 887 Congress St. Suite 400, Portland, ME 04102
Students should spend at least one half day at the office during the week. Timing should be arranged with your team.
Common diagnoses/cases:
- FEN
- Pyloric stenosis
- Hernias/hydroceles
- Rotational anomalies
- Appendicitis
- Anorectal malformations
- Biliary atresia
- Choledochal cysts
- Congenital diaphragmatic hernia
- Cryptorchidism
- Duodenal atresia
- Esophageal atresia / Tracheoesophageal fistula
- Gastroschisis / Omphalocele
- Hirschsprung's disease
- Intussusception
- Meckel’s diverticulum
- Neuroblastoma
- Necrotizing enterocolitis
- Tracheal / Esophageal foreign body
- Wilms tumor
- See this document for further details
SICU
SICU is an incredibly content dense rotation. Sometimes this can feel overwhelming however the approach to and management of critically ill patients is a fundamental part of surgical training. During this rotation you will become part of a busy surgical critical care team managing a wide variety of illnesses. The majority of patients are trauma patients however you will also see a number of general surgical and vascular patients as well. While on SICU you should respond to trauma activations (all level 1 and level 2 as able).
Your team: You will primarily work with the residents assigned to SICU. There is always a surgery resident however often you will be with anesthesia and EM residents as well. You will also work closely with APPs and pharmacists.
You should plan on taking on 1-2 patients as your own by the end of the week. Work with your residents on choosing which patients have educational value. You should treat these patients as your own- follow up on tests, procedures and check in with families.
Morning rounds are the epicenter of the SICU experience. You will be expected to perform a system based presentation of your patients during rounds.
During this rotation you will carry the Trauma pager. You should respond to any trauma that you are able to. You will also have time to attend trauma cases in the operating room.
Outpatient office: none
Common diagnoses/cases:
SICU
- Respiratory failure/ ventilator management
- Shock
- Procedures:
- Tracheostomy
- Percutaneous endoscopic gastrostomy (PEG)
- Central line
- Arterial line
- Chest tube
- Dressing changes
Trauma
- Exploratory laparotomy for trauma (eg splenectomy)
- Damage control surgery
- Neck exploration
- Cricothyroidotomy
- Resuscitative thoracotomy
- Chest tubes placement
- VATS
- Rib plating
Surgical Oncology
This is the primary service for the surgical management of malignancy. There is a very busy thyroid cancer practice (Dr. MacGillivray) but also a large volume of intra-abdominal and soft tissue oncologic surgery performed.
Outpatient office: 887 Congress St. Suite 400, Portland, ME 04102
Students should spend at least one half day at the office during the week. Timing should be arranged with your team.
Common diagnoses/cases:
- Thyroid cancer
- Parathyroid diseases
- Pancreatic cancer
- Whipple procedure
- Colon cancer
- Metastatic cancer
- Melanoma
- Sarcoma
- GIST
Thoracic
The thoracic service will expose you to a variety of benign and malignant thoracic diseases. It is a fairly small service but between the office and OR you will see a good variety of patients.
Outpatient office: 100 Campus Dr Suite 121, Scarborough, ME 04074
Students should spend at least one half day at the office during the week. Timing should be arranged with your team.
Common diagnoses/cases:
- Lung cancer
- GERD
- Hiatal hernia
- Esophageal cancer
- Esophagectomy
- VATS
- Thoracotomy
- Lung resections
Trauma
Your trauma exposure will be primarily be through your time on night float, in the SCU and on call. You should expect to see many trauma resuscitations and you should be able to participate in the primary/secondary survey in select patients.
Outpatient office: none
Common diagnoses/cases:
- Exploratory laparotomy for trauma (eg splenectomy)
- Damage control surgery
- Neck exploration
- cricothyroidotomy
- Resuscitative thoracotomy
- Chest tubes placement
- VATS
- Rib plating
Urology
The urology service offers exposure to a variety of urologic disease processes. You will be assigned to the resident team led by a chief resident who will coordinate your schedule.
Outpatient office:
Students should spend at least one half day at the office during the week. Timing should be arranged with your team.
Vascular
There are 2 busy vascular services in the hospital. You will be assigned to one of them with a group of vascular and general surgery residents. Expect to see numerous open and endovascular operations and participate on a busy inpatient service. You will have exposure to outpatient vascular patients during your office week.
Outpatient office: 92 Campus Dr Suite D, Scarborough, ME 04074
Students should spend at least one half day at the office during the week. Timing should be arranged with your team.
Common diagnoses/cases:
- Limb ischemia
- Angioplasty/stents
- Carotid disease ( carotid endarterectomy)
- Lower extremity bypass
- Aortoiliac occlusive disease
- AAA (open vs endovascular AAA repair)
